Long COVID Beyond the Acute Phase: Key Insights for General Practitioners
- Graham Exelby
- Sep 6, 2025
- 4 min read
Author: Based on original work by Dr Graham Exelby, revised by Dr Valerio Vittone (PhD), reviewed by Dr Jonathon Jenkins Date: September 05, 2025 Purpose: This summary simplifies the complex science of Long COVID for busy GPs, focusing on practical understanding, symptoms, and management implications. It draws from the original research paper to explain why symptoms persist and how to approach patients.
Abstract
Long COVID is more than just lingering symptoms after COVID-19—it's a ongoing condition involving inflammation, low oxygen levels (hypoxia), and overlapping body processes that keep the illness going. This paper describes it as progressing in three phases: an initial intense immune response, a middle stage of ongoing inflammation, and a chronic stage where low oxygen and scar-like changes cause lasting problems.
Key drivers include molecules like STAT3, CCL2, RAGE, NF-κB, HIF-1α, and the NLRP3 inflammasome, which create self-sustaining cycles of inflammation and damage. This explains common symptoms like extreme fatigue, worsening after activity (post-exertional malaise or PEM), brain fog, heart rate issues (dysautonomia), and stiff muscles or tissues.
For GPs: Recognize Long COVID as a treatable network of issues, not just "post-viral fatigue." Early intervention can break these cycles and prevent long-term damage like fibrosis or organ problems.
Introduction
When COVID-19 first hit in 2019, early treatments focused on blocking overactive immune cells (mast cells) with antihistamines (H1/H2 blockers) and low-dose naltrexone (LDN). These helped reduce severity in many cases. However, some patients—especially those with delayed treatment—develop harder-to-treat symptoms that last months or years.
Long COVID affects millions and isn't just from the virus itself. It's often linked to genetic factors that make inflammation harder to control. This paper proposes a "three-phase model" to explain how it evolves:
Acute Phase (first 4 weeks): Intense immune reaction ("cytokine storm") with leaky blood vessels and histamine release.
Transition Phase: Ongoing low-level inflammation and early brain drainage issues.
Chronic Phase: Low oxygen drives changes in metabolism, leading to scar tissue and persistent symptoms.
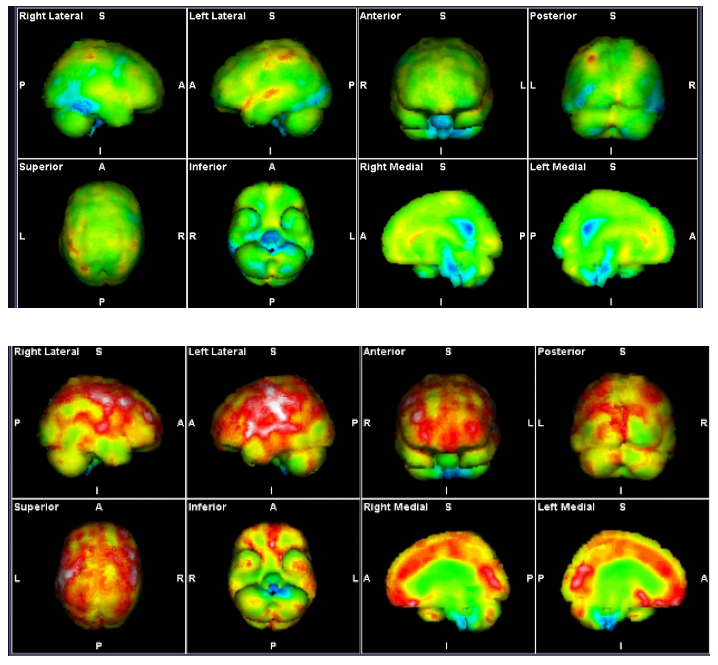
Brain scans (like SPECT) show reduced blood flow in areas like the brainstem, explaining symptoms like dizziness or cognitive issues. GPs should consider Long COVID in patients with ongoing fatigue or new symptoms after COVID-19, even mild cases.
How the Immune System Goes Wrong: The Cytokine Storm and "Histamine Bridge"
In the early infection, the virus triggers immune sensors (TLRs) on cells, leading to a flood of chemicals (cytokines like IL-6, TNF-α) that cause inflammation. Mast cells release histamine, worsening leaks in blood vessels and amplifying the response.
For GPs:
Symptoms to watch: Fever, shortness of breath, fatigue, rashes, or anxiety in acute phase.
Why it persists: In some, this doesn't switch off, leading to chronic issues. Genetic variations can make patients more prone.
Practical tip: Early use of antihistamines (e.g., cetirizine for H1, famotidine for H2) and LDN may help mild cases, but consult specialists for severe ones.
Key Players in Persistent Inflammation
STAT3: The Inflammation Switch
STAT3 is a protein that turns on genes for inflammation. In Long COVID, it's overactive due to cytokines like IL-6, leading to ongoing immune issues, blood vessel damage, and scar tissue (fibrosis) in muscles and organs.
Clinical link: Causes fatigue, brain fog, PEM, and stiff tissues (fascial changes).
For GPs: Patients may have overlapping conditions like POTS (postural orthostatic tachycardia syndrome) or fibromyalgia. Check for family history of autoimmune issues.
CCL2: The Cell Recruiter
CCL2 draws immune cells to inflamed areas, worsening damage. It's linked to brain inflammation and poor blood flow.
Symptoms: Head pressure, sensory sensitivity, muscle weakness.
Tip: Blood tests for inflammation markers (e.g., CRP, IL-6) can help identify active cases.
RAGE: The Damage Sensor
RAGE detects stress signals from damaged cells, keeping inflammation going. It contributes to leaky brain barriers and scar tissue.
Link to symptoms: Brain fog, dizziness, chronic pain.
GP note: Consider in patients with ongoing "allergic-like" symptoms post-infection.
NLRP3 Inflammasome: The Fire Starter
This complex senses danger and releases more inflammatory chemicals. It's central in chronic Long COVID, causing ongoing cell damage.
Other inflammasomes: AIM2 and NLRC4 may play roles too, especially with viral remnants.
Practical: Emerging treatments like colchicine (under trial) might target this, but not routine yet.
NF-κB: The Master Regulator
NF-κB controls many inflammatory genes. In the brain, it can protect neurons but inflame support cells (glia), leading to chronic issues.
Tip: Stress, infections, or poor diet can worsen this—advise lifestyle changes.
The Role of Low Oxygen (Hypoxia) and HIF-1α
As inflammation continues, tissues get less oxygen, stabilizing HIF-1α. This shifts energy production to inefficient modes, building up waste products like lactate, causing PEM and fatigue.
Brain effects: Reduced blood flow in key areas (seen on scans), leading to fog and autonomic problems.
Other loops: Kynurenine pathway increases brain excitation; succinate keeps HIF-1α active.
For GPs: Refer for brain imaging if symptoms suggest (e.g., persistent headaches). Oxygen therapies like HBOT may help in select cases.
The Vicious Cycle: Why Symptoms Don't Go Away
These factors form loops: Hypoxia → Damage signals → More inflammation → Worse hypoxia. This leads to scar tissue blocking drainage, worsening everything.
Common overlaps: POTS, ME/CFS, fibromyalgia—screen for these.
Risks: Long-term, could lead to neurodegeneration or organ damage.
Conclusion and Management Tips for GPs
Long COVID is a phased condition needing targeted approaches:
Acute: Stabilize mast cells (antihistamines, LDN).
Transition: Reduce inflammation (consider anti-inflammatories).
Chronic: Address hypoxia and scars (e.g., physical therapy, emerging drugs like tirzepatide or telmisartan—specialist referral).
Practical Advice:
Diagnosis: Use history, symptoms, and exclude other causes (blood tests, ECG).
Management: Multidisciplinary—PT, psychology, nutrition. Monitor for mental health impacts.
Future: Biomarker tests and trials may personalize treatment.
Patient Education: Explain it's real and treatable; encourage pacing to avoid PEM.
This is a hypothesis based on research—consult guidelines (e.g., NICE, CDC) for updates. References from original paper available on request.
Comments