Telmisartan and Candesartan in Mitigating Cognitive Impairment in Long COVID
- Graham Exelby
- May 26
- 13 min read
Updated: Jul 13
Dr Graham Exelby May 2024, revised May 2025
Abstract
Angiotensin II receptor blockers (ARBs), particularly telmisartan and candesartan, show promise in treating cognitive impairment in Long COVID by reducing brain inflammation, protecting blood vessels, and enhancing neuroplasticity.
We hypothesize that these ARBs can improve memory and executive function by targeting neuroinflammation and vascular dysfunction. Telmisartan’s superior brain penetration and PPAR-γ activation may offer broader benefits, while candesartan excels in long-term cognitive recovery. Their established safety in cardiovascular populations and preclinical evidence support their repurposing for Long COVID, with clinical trials urgently needed to validate efficacy.
Introduction
Cognitive impairment in Long COVID, characterized by memory loss, reduced executive function, and mental fatigue, poses a significant clinical challenge. Neuroimaging and molecular studies point to brain endothelial dysfunction, chronic neuroinflammation, glymphatic stagnation, and excitotoxic injury as key drivers. While no standard treatment exists, repurposing medications with targeted actions is a promising strategy.
Angiotensin II type 1 receptor blockers (ARBs), such as telmisartan and candesartan, offer multifaceted benefits beyond blood pressure control, including anti-inflammatory effects, blood-brain barrier (BBB) penetration, and modulation of microglial reactivity. Telmisartan’s longer half-life, lipophilicity, and PPAR-γ activation provide distinct neuroprotective advantages over candesartan. This paper reviews the pathophysiology of Long COVID cognitive impairment, compares the therapeutic potential of candesartan and telmisartan, and proposes future research directions to address this debilitating condition.
Pathophysiological Insights into Long COVID Cognitive Impairment
Long COVID-related cognitive dysfunction—often termed “brain fog”—is increasingly understood as a neurovascular–immune–metabolic disorder. Emerging evidence supports the convergence of the following pathological mechanisms:
Chronic Neuroinflammation and Glial Sensitization: SARS-CoV-2 triggers sustained activation of microglia and astrocytes via pattern recognition receptors (TLR4, RAGE), leading to NF-κB–mediated production of IL-1β, TNF-α, and CCL2. This feedback loop induces a state of central sensitization and impairs synaptic plasticity.
Cerebrovascular Dysfunction: Endothelial injury, microthrombi, and BBB disruption are common, driven by angiotensin II–induced vasoconstriction and oxidative stress. These alterations precipitate hypoperfusion, especially in the brainstem, basal ganglia, and frontal cortex—regions implicated in executive dysfunction.
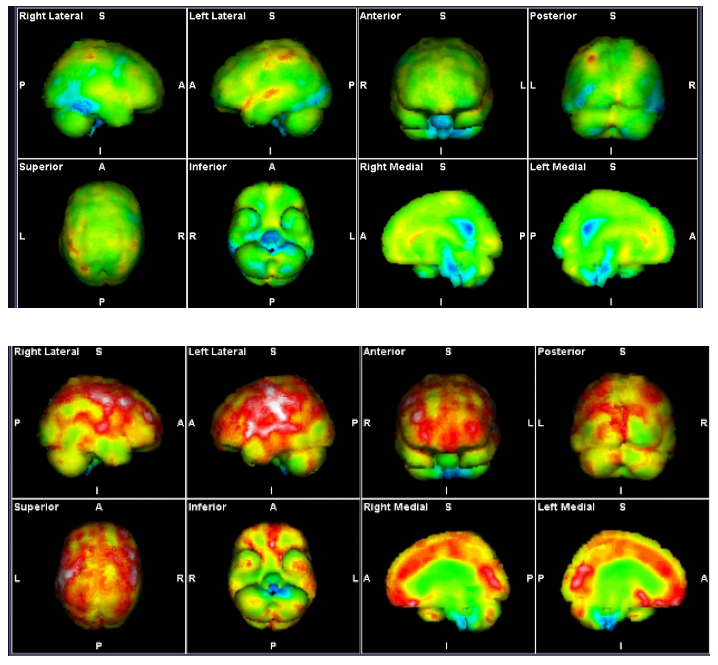
Glymphatic Stagnation: Disruption of perivascular clearance due to impaired aquaporin-4 (AQP4) function and venous congestion exacerbates neuroinflammatory burden. Standing-induced spreading hypoperfusion (as seen in SPECT studies) further impairs glymphatic efficiency.
Glutamate Excitotoxicity and GABA Dysregulation: Persistent neuroinflammation skews the GABA–glutamate balance, often observed in Long COVID patients with low GABA and aspartate, and elevated glutamate. This neurochemical profile contributes to cortical hyperexcitability and fatigue.
Mitochondrial Dysfunction and NAD⁺ Depletion: Viral persistence, oxidative stress, and PDH inhibition drive metabolic inflexibility. Nicotinamide riboside deficiency and impaired SIRT1/3 activation reduce neuronal resilience and repair capacity.
These mechanisms jointly underpin the cognitive deficits of Long COVID and suggest therapeutic targets: immune modulation (RAGE/TLR4/NF-κB), vascular stabilization, glutamate control, glymphatic flow restoration, and mitochondrial repair.
Additional Evidence from Alzheimer’s Disease Model
Further supporting telmisartan’s neuroprotective profile, a 2022 study by Torika et al.(21) using a mouse model of familial Alzheimer’s disease demonstrated that intranasal administration of telmisartan markedly reduced amyloid-β plaque burden, glial activation, and proinflammatory cytokine levels, while preserving neuronal integrity and improving spatial memory performance The intranasal route facilitated direct CNS access, bypassing the blood–brain barrier, and likely enhanced drug delivery to the glymphatic interface and autonomic brainstem nuclei.
Mechanistically, this effect was attributed to dual AT1R blockade (reducing NADPH oxidase–mediated ROS generation and downstream NF-κB signalling) and PPAR-γ activation, which enhanced mitochondrial resilience and microglial phenotypic switching. The pronounced suppression of TNF-α, IL-6, Iba-1, and GFAP, along with improvements in Morris water maze performance, aligns with telmisartan’s relevance in addressing neuroinflammation and cognitive impairment in Long COVID.
These findings substantiate telmisartan’s translational potential for neuroinflammatory syndromes beyond Alzheimer’s disease, particularly in contexts involving glymphatic congestion, central sensitization, and impaired waste clearance—core features of Long COVID cognitive decline. Notably, the authors proposed that intranasal delivery may enhance access to brainstem and perivascular lymphatic zones, offering mechanistic synergy with your ongoing glymphatic and lymphatic hypotheses in POTS and Long COVID. At this stage, we are using oral telmisartan and await research support for the intranasal delivery.
Mechanistic Insights on neuronal stabilization
Villapol et al. 2015 (6) demonstrated that both telmisartan and candesartan reduce neuronal apoptosis, glial reactivity, and lesion burden following traumatic brain injury (TBI), confirming their dual mechanism via AT1R blockade and PPARγ activation. Their study highlights the necessity of early intervention (within 6 hours post-injury), with both drugs failing to show benefit if delayed to 24 hours. Telmisartan excelled in early motor recovery, while candesartan offered more robust long-term cognitive benefits, underscoring potential for endotype-guided therapy.
Notably, direct anti-inflammatory effects on cultured glia (telmisartan blocked LPS-induced iNOS and IL-1β in microglia) were PPARγ-dependent. These findings strongly support the use of telmisartan in neuroinflammatory states with glial overactivation, such as Long COVID and POTS.
Glutamate Excitotoxicity and NR2B–PPARγ Signalling
Wang et al .2014 (19) described telmisartan’s protective role against glutamate-induced neurotoxicity via NR2B receptor modulation. This mechanism operates independently of AT1R, involving suppression of NR2B-associated signalling, inhibition of the JNK/c-Jun apoptotic axis, and preservation of mitochondrial integrity. Given the elevated glutamate and depleted GABA/aspartate profiles in many Long COVID and POTS patients, this PPARγ-dependent modulation of excitotoxic pathways represents a critical therapeutic target.
These findings provide molecular justification for telmisartan’s use in patients with redox imbalance, amino acid dysregulation, and central sensitization. They also extend its indications beyond vascular tone control toward glutamate–GABA system stabilization.
Telmisartan’s Expanded Role: Astrocyte–IL-6–STAT3 Axis Modulation
A 2024 study by Quan et al. significantly advances our understanding of telmisartan’s neuroimmune properties. Using a glioma–astrocyte co-culture model, low-dose telmisartan (5 μM) was shown to suppress astrocytic IL-6 production via PPAR-γ–dependent inhibition of NF-κB (p65) phosphorylation. This led to reduced STAT3 activation in adjacent glioma cells, which in turn downregulated pro-proliferative and migratory mediators such as Cyclin B1, MMP2, and MMP9.
These findings are relevant to Long COVID, where a persistent IL-6–STAT3 loop contributes to glial activation, cortical sensitization, and fatigue. Notably, telmisartan’s effects were independent of angiotensin II type 1 receptor blockade and were abrogated by a PPAR-γ antagonist. This supports a unique immunometabolic profile of telmisartan, targeting astrocyte-driven paracrine amplification in chronic neuroinflammation.
Such a mechanism may underlie telmisartan’s observed ability to reduce central fatigue and brainstem hypoperfusion, especially in patients with chronic IL-6 elevation and glymphatic dysfunction. Its glial-selective action supports use in neuroinflammatory states like Long COVID, ME/CFS, and POTS.
Therapeutic Potential of Candesartan and Telmisartan
Candesartan:
Neuroprotective Effects: Reduces neuroinflammation and amyloid-beta accumulation in preclinical models.
Cognitive Benefits: Improves cognitive performance in animal studies via modulation of the renin-angiotensin system (RAS) and attenuation of oxidative stress.
Telmisartan:
PPAR-γ Activation: Acts as a partial agonist of PPAR-γ, promoting anti-inflammatory and insulin-sensitizing effects.
Cognitive Enhancement: Upregulates brain-derived neurotrophic factor (BDNF) and its receptor TrkB in the hippocampus, improving learning and memory in hypertensive rat models.
Hypothesis:
We hypothesize that candesartan and telmisartan can improve cognitive impairment in Long COVID by addressing neuroinflammation, vascular dysfunction, and neuronal injury.
A 2020 study found that candesartan reduced hospital stay length in non-obese COVID-19 patients, though it did not address Long COVID or cognitive outcomes (1). No further evidence supports its continued use in this context. Given their established mechanisms, we propose candesartan and telmisartan as candidates for Long COVID cognitive impairment treatment, despite lacking TGA approval.
Co-morbidities and Mechanisms:
Co-morbidities like migraine, Alzheimer’s disease, stroke, and traumatic brain injury are critical in Long COVID management. Both ARBs:
Block angiotensin II type 1 receptor (AT1R), reducing excitotoxicity and oxidative damage via glutamate regulation (2).
Cross the BBB, enabling direct CNS effects to mitigate neuroinflammation (3).
Modulate microglial and astrocyte dysfunction, reducing inflammatory mediators like TNF-α and IL-1β (4, 5).
Protect against Alzheimer’s pathology by decreasing amyloid-beta and modulating glial activation (4, 5).
Potentially influence telomerase activity, reducing telomere shortening and cellular aging (12).
Traumatic Brain Injury and Comparative Efficacy
In traumatic brain injury (TBI) models, both ARBs reduce lesion volume, neuronal injury, and inflammation at non-hypotensive doses (0.1 mg/kg candesartan, 1 mg/kg telmisartan) (7). They protect cerebral blood flow and enhance recovery through AT1R blockade and PPAR-γ activation. Candesartan shows superior long-term cognitive benefits, while telmisartan excels in acute motor recovery (7). These effects are relevant to Long COVID’s neurovascular pathology.
Stroke
Telmisartan improves cerebral circulation in hypertensive patients with chronic stroke, maintaining blood flow despite blood pressure reduction, likely via PPAR-γ agonism and endothelial nitric oxide synthase (eNOS) upregulation (7, 10). Candesartan shares similar autoregulatory benefits.
Migraine
Candesartan is effective in migraine prophylaxis, likely by modulating CNS excitability, preserving BBB integrity, and reducing glutamate-induced excitotoxicity (11). Telmisartan’s potential in migraine is less studied but theoretically supported by its vascular and anti-inflammatory effects.
Intracranial Hypertension and Vascular Dynamics
Long COVID patients often exhibit brainstem hypoperfusion and hyperperfused brain SPECT findings, reflecting endotheliitis and BBB dysfunction. The glymphatic system, critical for cerebral waste clearance, is impaired in these conditions. ARBs may enhance glymphatic flow by reducing neuroinflammation and optimizing RAS-mediated fluid dynamics (7).
Telomerase Connection
Both ARBs may enhance telomerase activity, reducing telomere shortening in endothelial cells and potentially protecting against vascular and neuronal aging (12). Telmisartan’s PPAR-γ activation further supports these effects, offering cardiovascular and neuroprotective benefits.
Comparative Analysis
Candesartan and telmisartan share similarities but differ in key aspects, as summarized below:
Feature | Candesartan | Telmisartan |
Half-Life | 9-12 hours | 24 hours |
PPAR-γ Activation | Minimal (in vivo only) | Strong (partial agonist) |
BBB Penetration | Good | Superior (high lipophilicity) |
Cognitive Benefits | Stronger long-term | Stronger short-term |
Motor Recovery | Limited | Better in acute phase |
Unique Effects | TLR2 inhibition, amyloid-beta reduction | Metabolic regulation, BDNF upregulation |
Similarities: Both reduce lesion volume, neuronal injury, and inflammation in TBI models at non-hypotensive doses. They improve glymphatic flow and cerebral homeostasis via RAS modulation.
Differences: Telmisartan’s PPAR-γ activation and better BBB penetration enhance acute neuroprotection and metabolic regulation. Candesartan’s potent AT1R blockade and TLR2 inhibition favor long-term cognitive outcomes. No clinical trials directly compare them for Long COVID cognitive impairment.
Synergistic Potential of Telmisartan and Nicotinamide Riboside
Combining telmisartan with nicotinamide riboside (NR), a NAD⁺ precursor, targets multiple Long COVID pathways:
Mitochondrial Function: NR boosts NAD⁺ levels, activating SIRT1/SIRT3, while telmisartan enhances fatty acid oxidation via PPAR-γ.
Neuroinflammation: NR suppresses NF-κB, and telmisartan shifts microglia to an anti-inflammatory state.
Vascular Protection: Both upregulate eNOS, improving BBB integrity and glymphatic clearance.
Metabolic Regulation: NR activates AMPK, and telmisartan promotes insulin sensitivity.
This synergy supports clinical trials to explore dual-agent therapy for Long COVID cognitive impairment.
Evolving Pathophysiology in Long COVID: Telmisartan's Dual Role in Cytokine and Hypoxia Modulation
As Long COVID progresses, there appears to be a clinical transition from cytokine-dominant pathology to a hypoxia-dominant neurovascular impairment, particularly in patients with ongoing endothelial dysfunction, mast cell activation, and microvascular congestion. Telmisartan’s unique dual mechanism—as both an angiotensin II type 1 receptor (AT1R) blocker and partial peroxisome proliferator-activated receptor gamma (PPAR-γ) agonist—offers multifaceted benefits across this continuum.
1. Anti-Cytokine Action via PPAR-γ Agonism
PPAR-γ is a nuclear receptor that downregulates pro-inflammatory transcription pathways, including NF-κB. Telmisartan's selective PPAR-γ activity—confirmed in vitro by Benson et al. 2005 (16) attenuates TNF-α, IL-6, and CCL2, all of which are elevated in Long COVID and contribute to persistent glial activation, hippocampal dysfunction, and cortical sensitization.
This aligns with the findings of Ciavarella et al. 2021 (22), who proposed PPAR-γ agonists for cytokine storm mitigation, making telmisartan highly relevant in early- to mid-stage inflammatory Long COVID.
2. RAS Modulation and Vascular Repair
Telmisartan blocks the pathological arm of the renin-angiotensin system (angiotensin II → AT1R), which is amplified in SARS-CoV-2 due to ACE2 depletion. This blockade reduces vasoconstriction, microvascular oxidative stress, and sympathetic overactivation. Importantly, it also preserves endothelial function and may restore glymphatic and hippocampal perfusion.(Rothlin et al 2020 (23)
3. Synergy with Other Immune Modulators
Clinically, telmisartan could be co-administered with H1/H2 antihistamines and low-dose naltrexone (LDN). Antihistamines suppress mast cell–derived cytokines and reduce histamine-induced neurovascular permeability. LDN reduces glial priming via TLR4 antagonism and endorphin upregulation.
Telmisartan complements both: PPAR-γ agonism may inhibit mast cell–derived prostaglandin D2, while AT1R blockade mitigates hypoxia-induced RAGE ligand release.
4. Metabolic Regulation and Brain Energy Recovery
In chronic Long COVID, neuroenergetic deficits emerge due to PDH inhibition, NAD⁺ depletion, and impaired fatty acid oxidation. Telmisartan—via PPAR-γ activation—enhances mitochondrial biogenesis, boosts eNOS, and improves insulin sensitivity, synergizing well with nicotinamide riboside and magnesium to restore redox homeostasis and ATP availability.
Summary
Long COVID-related cognitive impairment is now recognized as a multifactorial syndrome driven by neuroinflammation, cerebral hypoperfusion, glymphatic stagnation, and mitochondrial dysfunction. Central to this is the chronic activation of glial cells via immune pathways such as TLR4 and RAGE, which drive excitotoxicity, BBB breakdown, and impaired synaptic function. Disruption in amino acid metabolism—including low GABA, aspartate, and ethanolamine with elevated glutamate—further contributes to neurocognitive decline and central sensitization.
Angiotensin II receptor blockers (ARBs), particularly candesartan and telmisartan, offer mechanistically aligned therapeutic potential. Both agents improve cerebral perfusion and reduce inflammation at non-hypotensive doses by blocking AT1R signalling.
Telmisartan’s strong blood-brain barrier penetration and partial PPAR-γ agonism uniquely enable it to modulate mitochondrial function, suppress NF-κB and CCL2 activity, and enhance neurotrophic support via BDNF.
Candesartan, while less metabolically active, provides robust long-term neuroprotection, including amyloid-beta modulation and TLR2 inhibition, relevant to patients with overlapping neurodegenerative risk.
The combination of telmisartan with nicotinamide riboside may amplify benefits by restoring NAD⁺ levels, enhancing SIRT activity, and reversing neuroenergetic deficits. Given their safety and pleiotropic actions, these ARBs are promising candidates for clinical trials in Long COVID cognitive impairment, with telmisartan emerging as a particularly well-suited first-line agent.
Conclusion
Telmisartan and candesartan offer compelling therapeutic potential for mitigating cognitive impairment in Long COVID through pleiotropic neurovascular and immune-modulating mechanisms. While both ARBs exert anti-inflammatory and endothelial-protective effects, telmisartan’s unique PPAR-γ agonist activity confers additional benefits by directly suppressing astrocyte-derived IL-6 and downstream STAT3 signalling—critical mediators of glial-driven neuroinflammation and cortical sensitization.
Recent evidence from glioma–astrocyte co-culture models (Quan et al., 2024) demonstrates that low-dose telmisartan exerts a glial-selective, paracrine-modulating effect that is independent of AT1R blockade. This supports its utility in neuroimmune conditions such as Long COVID, ME/CFS, and POTS, where persistent IL-6/STAT3 loops, mitochondrial dysfunction, and glymphatic congestion are key pathological features.
Given its strong BBB permeability, metabolic advantages, and mechanistic relevance across multiple Long COVID endotypes, telmisartan emerges as a promising first-line ARB candidate—particularly when combined with agents like nicotinamide riboside for mitochondrial restoration. Urgent biomarker-guided trials are warranted to evaluate its efficacy in reversing neuroinflammatory signatures and improving cognitive outcomes in affected patients.
References:
Lukito AA, Widysanto A, Lemuel TAY, Prasetya IB, Massie B, Yuniarti M, Lumbuun N, Pranata R, Meidy C, Wahjoepramono EJ, Yusuf I. Candesartan as a tentative treatment for COVID-19: A prospective non-randomized open-label study. Int J Infect Dis. 2021 Jul;108:159-166. doi: 10.1016/j.ijid.2021.05.019. Epub 2021 May 24. PMID: 34038766; PMCID: PMC8142270.
Fujita T, Hirooka K, Nakamura T, Itano T, Nishiyama A, Nagai Y, Shiraga F. Neuroprotective effects of angiotensin II type 1 receptor (AT1-R) blocker via modulating AT1-R signaling and decreased extracellular glutamate levels. Invest Ophthalmol Vis Sci. 2012 Jun 26;53(7):4099-110. doi: 10.1167/iovs.11-9167. PMID: 22661470.
Weatherston, A. Candesartan potential therapeutic for Alzheimer’s disease. Neuro Central. 2016. https://www.neuro-central.com/potential-role-of-candesartan-in-alzheimers-treatment/
Zheng, M., Karki, R., Williams, E.P. et al. TLR2 senses the SARS-CoV-2 envelope protein to produce inflammatory cytokines. Nat Immunol 22, 829–838 (2021). https://doi.org/10.1038/s41590-021-00937-x
Torika N, Asraf K, Apte RN, Fleisher-Berkovich S. Candesartan ameliorates brain inflammation associated with Alzheimer's disease. CNS Neurosci Ther. 2018 Mar;24(3):231-242. doi: 10.1111/cns.12802. Epub 2018 Jan 24. PMID: 29365370; PMCID: PMC6489976.
Torika N, Asraf K, Danon A, Apte RN, Fleisher-Berkovich S. Telmisartan Modulates Glial Activation: In Vitro and In Vivo Studies. PLoS One. 2016 May 17;11(5):e0155823. doi: 10.1371/journal.pone.0155823. PMID: 27187688; PMCID: PMC4871324.
Villapol S, Balarezo MG, Affram K, Saavedra JM, Symes AJ. Neurorestoration after traumatic brain injury through angiotensin II receptor blockage. Brain. 2015 Nov;138(Pt 11):3299-315. doi: 10.1093/brain/awv172. Epub 2015 Jun 26. PMID: 26115674; PMCID: PMC4731413.
Pelliccia F, Pasceri V, Cianfrocca C, Vitale C, Speciale G, Gaudio C, Rosano GM, Mercuro G. Angiotensin II receptor antagonism with telmisartan increases number of endothelial progenitor cells in normotensive patients with coronary artery disease: a randomized, double-blind, placebo-controlled study. Atherosclerosis. 2010 Jun;210(2):510-5. doi: 10.1016/j.atherosclerosis.2009.12.005. Epub 2009 Dec 11. PMID: 20044087.
Stierschneider A, Wiesner C. Shedding light on the molecular and regulatory mechanisms of TLR4 signaling in endothelial cells under physiological and inflamed conditions. Front Immunol. 2023 Nov 24;14:1264889. doi: 10.3389/fimmu.2023.1264889. PMID: 38077393; PMCID: PMC10704247.
Saavedra JM, Benicky J, Zhou J . Mechanisms of the anti-ischemic effect of angiotensin II AT(1) receptor antagonists in the brain. Cell Mol Neurobiol 2006; 26: 1099–1111.
Sprenger T, Viana M, Tassorelli C. Current Prophylactic Medications for Migraine and Their Potential Mechanisms of Action. Neurotherapeutics. 2018 Apr;15(2):313-323. doi: 10.1007/s13311-018-0621-8. PMID: 29671241; PMCID: PMC5935650.
Yi W, Chen F, Zhang H, Tang P, Yuan M, Wen J, Wang S, Cai Z. Role of angiotensin II in aging. Front Aging Neurosci. 2022 Dec 2;14:1002138. doi: 10.3389/fnagi.2022.1002138. PMID: 36533172; PMCID: PMC9755866.
Zhang X, Dong Y, Dong H, Cui Y, Du Q, Wang X, Li L, Zhang H. Telmisartan Mitigates TNF-α-Induced Type II Collagen Reduction by Upregulating SOX-9. ACS Omega. 2021 Apr 22;6(17):11756-11761. doi: 10.1021/acsomega.1c01170. PMID: 34056329; PMCID: PMC8154015.
Kurokawa H, Sugiyama S, Nozaki T, Sugamura K, Toyama K, Matsubara J, Fujisue K, Ohba K, Maeda H, Konishi M, Akiyama E, Sumida H, Izumiya Y, Yasuda O, Kim-Mitsuyama S, Ogawa H. Telmisartan enhances mitochondrial activity and alters cellular functions in human coronary artery endothelial cells via AMP-activated protein kinase pathway. Atherosclerosis. 2015 Apr;239(2):375-85. doi: 10.1016/j.atherosclerosis.2015.01.037. Epub 2015 Jan 31. PMID: 25682036.
Honda A, Matsuura K, Fukushima N, Tsurumi Y, Kasanuki H, Hagiwara N. Telmisartan induces proliferation of human endothelial progenitor cells via PPARgamma-dependent PI3K/Akt pathway. Atherosclerosis. 2009 Aug;205(2):376-84. doi: 10.1016/j.atherosclerosis.2008.12.036. Epub 2008 Dec 31. PMID: 19193378.
Sariol, A., Perlman, S. SARS-CoV-2 takes its Toll. Nat Immunol 22, 801–802 (2021). https://doi.org/10.1038/s41590-021-00962-w
Benson,S et al. Identification of Telmisartan as a Unique Angiotensin II Receptor Antagonist With Selective PPARγ–Modulating Activity. Hypertension, 2004. https://doi.org/10.1161/01.HYP.0000123072.34629.57
Uehara G, Takeda H. Relative effects of telmisartan, candesartan and losartan on alleviating arterial stiffness in patients with hypertension complicated by diabetes mellitus: an evaluation using the cardio-ankle vascular index (CAVI). J Int Med Res. 2008 Sep-Oct;36(5):1094-102. doi: 10.1177/147323000803600529. PMID: 18831906.
Zhang P, Hou Y, Tu W, Campbell N, Pieper AA, Leverenz JB, Gao S, Cummings J, Cheng F. Population-based discovery and Mendelian randomization analysis identify telmisartan as a candidate medicine for Alzheimer's disease in African Americans. Alzheimers Dement. 2023 May;19(5):1876-1887. doi: 10.1002/alz.12819. Epub 2022 Nov 4. PMID: 36331056; PMCID: PMC10156891.
Wang J, Pang T, Hafko R, Benicky J, Sanchez-Lemus E, Saavedra JM. Telmisartan ameliorates glutamate-induced neurotoxicity: roles of AT(1) receptor blockade and PPARγ activation. Neuropharmacology. 2014 Apr;79:249-61. doi: 10.1016/j.neuropharm.2013.11.022. Epub 2013 Dec 4. PMID: 24316465; PMCID: PMC3950310.
Stierschneider A, Wiesner C. Shedding light on the molecular and regulatory mechanisms of TLR4 signaling in endothelial cells under physiological and inflamed conditions. Front Immunol. 2023 Nov 24;14:1264889. doi: 10.3389/fimmu.2023.1264889. PMID: 38077393; PMCID: PMC10704247.
Torika, N., Asraf, K., Cohen, H., Fleisher-Berkovich, S., Intranasal Telmisartan Ameliorates Brain Pathology in Five Familial Alzheimer's Disease Mice, Brain, Behavior, and Immunity (2017), doi: http://dx.doi.org/10.1016/j.bbi.2017.04.001
Ciavarella C, Motta I, Valente S, Pasquinelli G. Pharmacological (or Synthetic) and Nutritional Agonists of PPAR-γ as Candidates for Cytokine Storm Modulation in COVID-19 Disease. Molecules. 2020 Apr 29;25(9):2076. doi: 10.3390/molecules25092076. PMID: 32365556; PMCID: PMC7248959.
Rothlin RP, Pelorosso FG, Duarte M, et al. Telmisartan and losartan: The marked differences between their chemical and pharmacological properties may explain the difference in therapeutic efficacy in hospitalized patients with COVID-19. Pharmacol Res Perspect. 2023;11(2):e01083. doi:10.1002/prp2.1083
Wei Quan, Cheng-Shi Xu, Chao Ma, Xi Chen, Dong-Hu Yu, Zhi-Yu Li, Dan-Wen Wang, Feng Tang, Gui-Ping Wan, Jing Wan, Ze-Fen Wang, Zhi-Qiang Li. Anti-tumor effects of telmisartan in glioma-astrocyte non-contact co-cultures: A critical role of astrocytic IL-6-mediated paracrine growth promotion. International Immunopharmacology. 2024. https://doi.org/10.1016/j.intimp.2024.112707.
Pang T, Wang J, Benicky J, Sánchez-Lemus E, Saavedra JM. Telmisartan directly ameliorates the neuronal inflammatory response to IL-1β partly through the JNK/c-Jun and NADPH oxidase pathways. J Neuroinflammation. 2012 May 29;9:102. doi: 10.1186/1742-2094-9-102. PMID: 22642771; PMCID: PMC3410820.


Comments