POTS Symptoms Overview
- Graham Exelby
- May 27, 2025
- 7 min read
Updated: May 30, 2025
Dr Graham Exelby May 2025
Introduction
Chronic multisystem conditions such as Postural Orthostatic Tachycardia Syndrome (POTS), Long COVID, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), and fibromyalgia present with heterogeneous symptom profiles that have long eluded precise mechanistic categorization. Historically, these symptoms have been treated as disparate manifestations rather than coherent indicators of systemic dysfunction.
However, emerging evidence—drawn from molecular biology, neuroimmunology, metabolomics, and hemodynamic studies—suggests that these syndromes share overlapping pathophysiological endotypes. These include dysregulated immune signalling, impaired autonomic control, mitochondrial dysfunction, and structural or hydraulic anomalies, particularly involving cerebral perfusion and venous outflow.
In this context, symptoms such as fatigue, brain fog, orthostatic intolerance, post-exertional malaise, and pain should no longer be seen as isolated clinical descriptors but as downstream reflections of interrelated disturbances in immunologic, autonomic, metabolic, and mechanical axes. For instance, low-grade neuroinflammation mediated by RAGE and inflammasome activation may synergize with mitochondrial oxidative stress, impairing pyruvate dehydrogenase (PDH) activity and reducing cerebral energy availability. Simultaneously, preload failure and intracranial venous congestion may compound central hypoperfusion and contribute to progressive autonomic destabilization. Amino acid imbalances—particularly low aspartate, glutamine, and GABA alongside elevated glutamate—further implicate disrupted neurotransmission and impaired anaplerosis (metabolic process of replenishing the intermediates of a biochemical cycle, especially the citric acid cycle) in sustaining symptom clusters.
By mapping common symptoms to these interwoven pathophysiological threads, a more integrated model of disease emerges—one that not only improves diagnostic clarity but also paves the way for precision-targeted therapeutics. This paper proposes a unified framework in which symptoms are reinterpreted through the lens of converging dysfunctions across immune, autonomic, metabolic, and mechanical systems, with the aim of transforming clinical assessment and guiding individualized intervention strategies.
POTS as a Core Autonomic Disorder
Postural Orthostatic Tachycardia Syndrome (POTS) can be conceptualized as a disorder of autonomic instability with substantial pathophysiological overlap with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME), Long COVID, Fibromyalgia, Gulf War Syndrome and other post-viral syndromes. While POTS is often distinguished by its hallmark orthostatic intolerance and cardiovascular dysregulation, its broader symptomatology—severe fatigue, cognitive dysfunction (“brain fog”), and post-exertional malaise (PEM)—mirrors that of CFS/ME. The mechanistic underpinnings of POTS appear multifactorial, involving metabolic dysfunction, preload failure, intracranial hypertension (ICH), and progressive brainstem hypoperfusion, all of which converge to impair autonomic regulation. Brainstem dysfunction, in particular, is emerging as a central unifying factor in POTS, given its role in coordinating baroreflex function, cerebral autoregulation, and immune signalling.
Neuroimmune Dysregulation: The TLR4/NF-κB/RAGE Axis in POTS
Chronic neuroinflammation and immune dysfunction combines in the pathophysiology of POTS, with the TLR4/NF-κB/RAGE (Receptor for Advanced Glycation End-products) axis serving as a critical driver. Toll-like receptor 4 (TLR4) activation, often in response to viral infections, bacterial endotoxins, or sterile inflammatory stimuli, triggers a downstream cascade via NF-κB, a transcription factor that upregulates the expression of pro-inflammatory cytokines (IL-6, TNF-α, and IL-1β). This sustained inflammatory response exacerbates endothelial dysfunction, contributing to vasomotor instability and blood-brain barrier (BBB) disruption. RAGE activation, particularly in response to oxidative stress and glycation end-products, amplifies this inflammatory signalling, promoting a vicious cycle of neuroinflammation, microglial activation, and autonomic dysregulation.
The brainstem, particularly the medullary autonomic centres, is highly susceptible to these inflammatory and ischaemic insults. Chronic NF-κB activation within the brainstem contributes to glial priming, mitochondrial dysfunction, and maladaptive autonomic responses, leading to sympathetic hyperactivity, impaired baroreflex sensitivity, and dysregulated cerebral autoregulation.
Metabolic Dysfunction, Mitochondrial Collapse, and Post-Exertional Malaise
Post-exertional malaise (PEM) in POTS represents a metabolic collapse triggered by immune activation, autonomic dysfunction, and energy depletion. Key metabolic disruptions include pyruvate dehydrogenase (PDH) dysfunction, amino acid depletion (notably aspartate and glutamate imbalances), and impaired oxidative phosphorylation, leading to inefficient ATP production and exacerbated fatigue. In particular, excessive RAGE/NF-κB activation impairs mitochondrial function by increasing oxidative stress and altering redox homeostasis, further depleting energy reserves. This fragile energetic state is easily overwhelmed by exertion, precipitating a crash that is both neuroinflammatory and metabolic in nature.
Central Sensitization and Dysautonomia
Beyond immune-metabolic dysfunction, central sensitization plays a significant role in the pain, fatigue, and autonomic disturbances seen in POTS. Chronic activation of glial cells and neuroinflammatory pathways increases the excitability of pain-processing networks and autonomic circuits, leading to widespread hypersensitivity to stimuli, exaggerated autonomic responses, and persistent fatigue. This process is particularly relevant in POTS patients with comorbid hypermobility spectrum disorders (HSD) or Ehlers-Danlos Syndrome (EDS), as connective tissue abnormalities may exacerbate mechanical instability and neuroimmune activation.
Unifying Mechanisms and Future Directions
The association between POTS and CFS/ME is well-documented, with autonomic dysfunction, immune dysregulation, and mitochondrial impairment serving as shared features. Small-scale tilt table studies indicate orthostatic intolerance in over 90% of CFS/ME patients, further reinforcing the notion that these conditions exist on a pathophysiological spectrum rather than as distinct entities. Genetic predisposition, viral or post-infectious triggers, and connective tissue abnormalities appear to be key risk factors, influencing the severity and trajectory of disease progression.
By recognizing the unifying roles of brainstem hypoperfusion, TLR4/NF-κB/RAGE-driven neuroinflammation, mitochondrial dysfunction, and metabolic collapse, targeted interventions can be refined to address both the autonomic and immune components of POTS. Potential therapeutic strategies include SIRT4 modulation (to restore mitochondrial function), anti-inflammatory interventions, and metabolic support therapies aimed at mitigating PEM and restoring autonomic stability. The recognition of the role of the various mechanistic “drivers” such as Nutcracker, may-Thurner, Stylohyoid, Thoracic Outlet Syndromes, the role of posture, EDS and neck trauma provide insights into managing the autonomic and inflammatory chaos, and a springboard into management of POTS by treating causes, rather than medication to control symptoms.
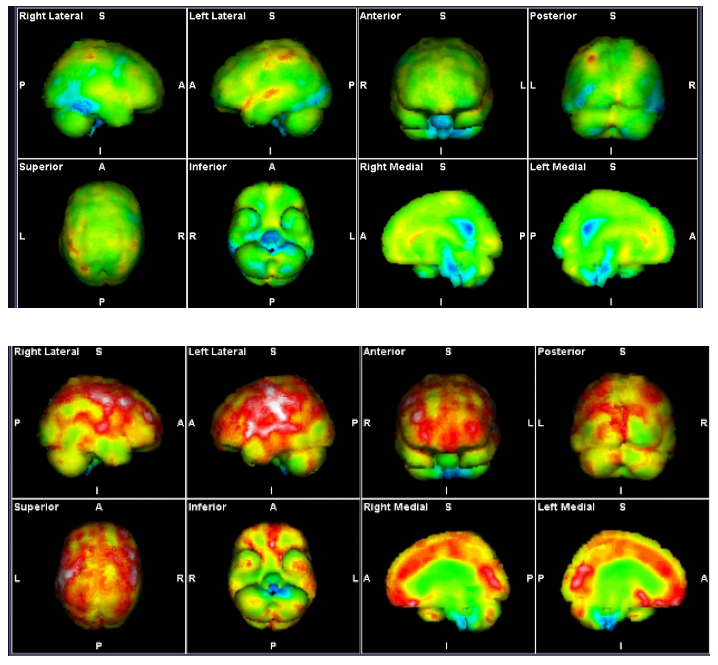
Figure 1. Comparison of Symptoms Severity among POTS, FMS, GWS and Long COVID
CFS rating is 10/10 in fatigue and PEM.

CFS Diagnostic Criteria -NICE Guidelines 2021-all symptoms are required for diagnosis (279)
Debilitating fatigue that is worse with activity, is not caused by excessive cognitive, physical, emotional or social exertion, and is not significantly relieved by rest.
Post exertional malaise after activity in which the worsening of symptoms:
Is often delayed in onset by hours or days
Is disproportionate to the activity
Has a prolonged recovery time that may last hours, days, weeks or longer
Unrefreshing sleep or sleep disturbance, or both, which may include:
feeling exhausted, feeling flu-like or stiff on waking
broken or shallow, altered sleep pattern or hypersomnia hypersomnia
Cognitive difficulties (sometimes described as 'brain fog'), which may include problems finding words or numbers, difficulty in speaking, slowed responsiveness, short-term memory problems and difficulty concentrating or multitasking.
The symptoms persistent for at least three months
Symptoms:
These will dealt with individually looking at the pathophysiology and potential solutions.
Neurological and Cognitive Symptoms
Neurological and cognitive symptoms in POTS, Long COVID, and related syndromes reflect a dynamic interplay of brainstem hypoperfusion, neuroimmune activation, and excitatory-inhibitory imbalance. Microglial priming and glutamate excitotoxicity, particularly in the locus coeruleus and limbic circuits, drive hypervigilance, anxiety, and disrupted sleep architecture. Simultaneously, low GABA and aspartate levels, as observed in urinary amino acid profiles, compromise cortical inhibition and cognitive flexibility.
Treatment strategies often involve metabolic repletion (e.g., nicotinamide riboside), low-dose naltrexone, and neurostabilization with H1/H2 blockers to reduce limbic overdrive and improve cerebral autoregulation. Simple treatments involving improved posture to improve brainstem perfusion while the more complex mechanical, vascular and lymphatic are vital
Cognitive dysfunction ("brain fog")
Central sensitization
Visual aberrations (blurred vision, photophobia)
Tinnitus
Non-epileptiform seizures
Syncope and pre-syncope
Sleep dysfunction (non-restorative sleep, hypersomnia, sleep–wake dysregulation)
Emotional lability / anxiety (neuroimmune–limbic interplay)
Cardiovascular and Autonomic Symptoms
Autonomic symptoms arise from a convergence of preload failure, baroreceptor dysfunction, and impaired sympathetic-parasympathetic coordination. Central mechanisms involve brainstem hypoxia, while peripheral drivers include venous congestion (e.g., Nutcracker syndrome, May-Thurner), thoracic outlet syndrome, MALS, SMA and spinal-driven dysfunction affecting sympathetic afferents and EDS-associated vascular laxity. Sympathetic activation from lymphatic dysfunction is a probable significant contributor. The “functional continuum” between the brainstem hypoxia- parasympathetic dysregulation with the spinal afferents, cardiac and coeliac plexus and ganglia complete the autonomic dysregulation.
Interventions such as management of faecal loading, salt/fluid loading, abdominal compression, and mitochondrial cofactors target the underlying haemodynamic and metabolic derangements, while addressing baroreflex dysfunction usually require physical interventions. Acupuncture (particularly the Kiiko-Matsumoto style can play a vital role in stabilizing the autonomics before physical interventions can be commenced.
Fatigue
Post-exertional malaise
Exercise intolerance
Palpitations (especially in orthostatic stress)
Chest pain (atypical or exertion-triggered)
Shortness of breath
Orthostatic intolerance (lightheadedness, dizziness)
Temperature dysregulation
Heat intolerance
Sweating dysfunction
Raynaud’s phenomenon
Faecal loading
Abdominal pain and tachycardia when eatingHypovolemia / thirst dysregulation (volume dysregulation axis)
Structural, Mechanical, and Circulatory Symptoms
Mechanical and structural contributors to POTS symptoms include intracranial hypertension, cervical instability, venous and lymphatic outflow obstruction—each worsening brainstem perfusion, altering intracranial head pressure and autonomic coherence. Loss of cervical lordosis, vertebral venous reflux, and CSF canalicular compression further compromise neurovascular flow. Recognition of these factors allows for non-pharmacologic recovery through postural correction and targeted physical, lymphatic and myofascial therapies, in parallel with hydraulic decompression (e.g., manual lymphatic drainage).
Intracranial hypertension
Coat hanger pain (neck and shoulder)
Arm pain
Leg pain
Intolerance of altitude change
Menstrual irregularities (dysautonomia–hypothalamic axis dysfunction)
Immune–Inflammatory and Mast Cell–Associated Symptoms
Mast cell activation and immune hypersensitivity are central to the symptom burden in POTS and Long COVID, particularly in chemically sensitive or histamine-reactive patients. The RAGE/TLR4/NFKB/CCL2 axis, ethanolamine depletion, and dysbiosis-related gut–immune–brain signalling drive chronic low-grade inflammation.
Initial stabilization often requires dual H1/H2 antihistamines, mast cell modulators (e.g., cromolyn), and dietary reduction of histaminergic triggers. In cases of sustained dysregulation, therapies targeting CCL2, nicotinamide metabolism, or immunoglobulin rebalancing may be required.
Mast cell activation (flushing, urticaria, histamine intolerance)
GI symptoms (nausea, dysmotility, bloating, early satiety)
Urinary symptoms (urgency, frequency, retention)
Allergic-like reactivity (pseudoallergic responses, chemical sensitivities)
Conclusion
Postural Orthostatic Tachycardia Syndrome (POTS) represents a multisystem dysregulatory disorder in which symptoms are not discrete clinical features but converging reflections of deeper pathophysiological failures. The unifying thread across fatigue, cognitive dysfunction, post-exertional malaise, orthostatic intolerance, and pain lies in progressive brainstem hypoperfusion—driven by impaired venous and lymphatic outflow, reduced cerebrovascular autoregulation, and metabolic collapse. This is further amplified by immune activation via the TLR4/NF-κB/RAGE axis, mitochondrial dysfunction, PDH inhibition, and profound amino acid derangements including low GABA, glutamine, and aspartate.
Mechanistically, this landscape demands a paradigm shift from symptomatic treatment to upstream restoration of cerebral perfusion, autonomic coherence, and immune balance. Central to this are structural and mechanical corrections—targeting cervical lordosis, venous compression syndromes (e.g., Nutcracker, May-Thurner), thoracic outlet obstruction, and intracranial hypertension—alongside recognition of spinal afferent contributions and the “functional continuum” linking brainstem, cardiac, and coeliac plexuses.
Interventions must therefore be layered and individualized: from positional therapies and lymphatic decompression, to mitochondrial support (e.g., nicotinamide riboside), immune modulation (e.g., H1/H2 blockade, low-dose naltrexone), and, where required, immune rebalancing with IVIG. Recognition of faecal loading, mast cell activation, and gut–brain–immune cross-talk further enables tailored approaches that address not only autonomic instability but the immune-metabolic terrain sustaining it.
This integrated model recasts POTS as a remediable dysfunction—not an idiopathic syndrome—unlocking a path forward through root-cause resolution, targeted metabolic repair, and anatomical decompression. The future of POTS management lies in decoding the body’s layered compensatory failures and restoring balance across neurovascular, immune, metabolic, and mechanical domains.

Comments